Introduction
Clean claim submission is the foundation of effective medical billing. It refers to claims that are submitted accurately, completely, and in full compliance with payer requirements on the first attempt. These claims have no errors in patient demographics, coding, or documentation, allowing them to process smoothly through payer systems without delays or rejections.
The importance of clean claim submission goes beyond just administrative efficiency. Healthcare providers who consistently submit clean claims enjoy benefits such as:
- Faster reimbursement cycles
- Reduced administrative workload
- Improved performance in managing revenue cycles
Clean claims directly lead to better cash flow, fewer denied claims, and less time spent by staff on rework and resubmissions.
Understanding Clean Claim Submission
A clean claim definition encompasses a medical billing submission that contains accurate, complete, and compliant information meeting all payer requirements without requiring additional documentation or corrections. These claims pass through payer systems seamlessly, triggering immediate processing and payment without delays or rejections.
Essential Components of Clean Claims
Clean claims must satisfy three fundamental criteria:
- Accuracy: Patient demographics, provider information, and service details match exactly across all documentation
- Completeness: All required fields contain appropriate data, including diagnosis codes, procedure codes, and supporting documentation
- Payer Compliance: Submission adheres to specific insurance carrier guidelines, formatting requirements, and coverage policies
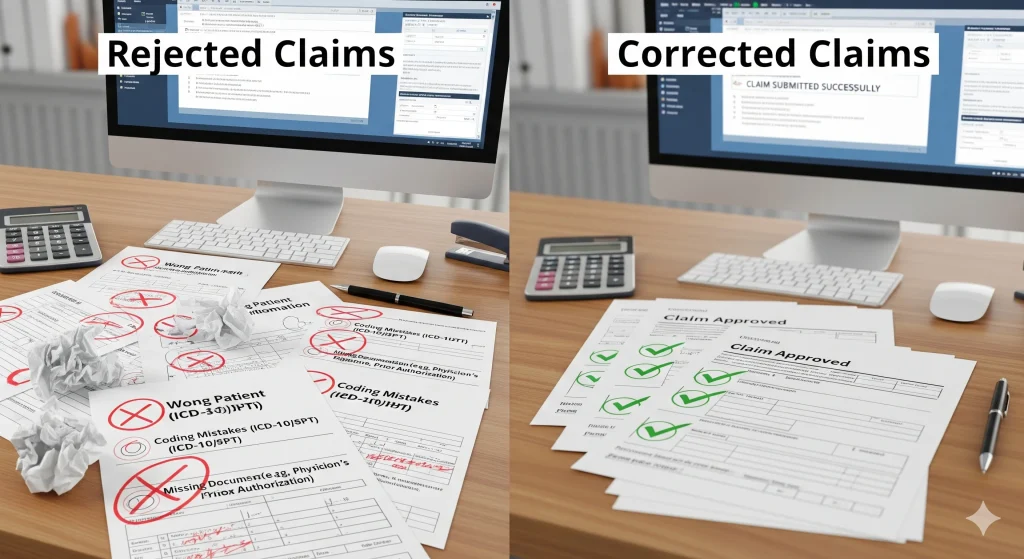
Common Medical Claims Errors
Several recurring issues prevent claims from achieving a clean status:
Patient Information Discrepancies
- Incorrect insurance member IDs or policy numbers
- Mismatched patient names or birthdates
- Outdated insurance coverage details
Coding Mistakes
- Inappropriate ICD-10 diagnosis code for documented conditions
- Incorrect CPT procedure codes for services rendered
- Missing or invalid modifier usage
Documentation Deficiencies
- Insufficient clinical notes supporting billed services
- Missing prior authorization numbers when required
- Incomplete referral documentation for specialist visits
Documentation and Coding Accuracy
Precise clinical documentation serves as the foundation for clean claim submission. Providers must ensure their medical records comprehensively support every billed service with appropriate detail and medical necessity justification. Certified coders then translate this documentation into standardized codes that accurately reflect the care provided while meeting payer requirements for reimbursement.
The Importance of Clean Claim Submission in Medical Billing
Clean claim submission is crucial for effective revenue cycle management. It directly affects a healthcare provider’s financial stability and operational efficiency. When claims are submitted correctly the first time, they move through the payer approval process without delays or rejections.
Faster Reimbursement Cycles Transform Cash Flow
Healthcare providers experience significantly improved cash flow when claims are processed without interruption. Clean claims typically receive payment within 14 -30 days, compared to denied or rejected claims that can take 60-90 days or longer to resolve. This acceleration in payment cycles allows practices to:
- Maintain consistent operational funding
- Reduce reliance on credit lines or loans
- Invest in practice improvements and equipment upgrades
- Meet payroll and vendor obligations without financial strain
Reduced Denials Minimize Administrative Burden
Clean claims dramatically decrease the volume of denials requiring staff intervention. Each denied claim demands approximately 30-45 minutes of administrative work to research, correct, and resubmit. When practices maintain high clean claim rates, their billing teams can focus on proactive revenue cycle activities rather than reactive denial management.
Compliance in Billing Protects Practice Integrity
Accurate claim submission ensures adherence to federal regulations and payer-specific requirements. Consistent compliance reduces the risk of audits, financial penalties, and potential fraud allegations. Healthcare providers who prioritize clean claims demonstrate their commitment to ethical billing practices while protecting their reputation and avoiding costly regulatory interventions.
Operational Benefits of Maintaining High Clean Claim Rates
High clean claim rates create a ripple effect of operational efficiency throughout healthcare organizations. When claims process smoothly on first submission, revenue cycle management becomes predictable and systematic. Administrative teams spend less time tracking rejected claims, researching denial reasons, and coordinating resubmissions. This streamlined workflow allows staff to focus on proactive tasks rather than reactive problem-solving.
The financial impact of administrative cost reduction becomes evident through decreased labor hours dedicated to claim corrections. Healthcare organizations typically spend 60-80% more time processing denied claims compared to clean submissions. Each denied claim requires:
- Research into denial reasons and payer requirements
- Coordination between clinical and billing teams
- Documentation gathering and claim resubmission
- Extended follow-up communications with payers
Clean claims eliminate these resource-intensive activities, allowing organizations to process higher claim volumes with existing staff levels. The cost savings extend beyond labor expenses to include reduced postage, phone calls, and system processing fees associated with multiple submission attempts.
Staff burnout decreases significantly when billing teams work with efficient processes. Repetitive denial management tasks create frustration and job dissatisfaction among administrative personnel. Clean claim processes provide staff with measurable success metrics and reduce the stress associated with constant problem resolution. This improved work environment leads to better employee retention and enhanced workforce productivity across the entire revenue cycle operation.
Furthermore, integrating advanced technologies such as artificial intelligence into the claims process can further enhance operational efficiency. AI can automate routine tasks, analyze vast amounts of data for quicker decision-making, and even predict potential claim denials based on historical trends. This not only alleviates the administrative burden but also significantly improves financial performance by reducing errors and increasing the speed of claim processing.
Strategies to Improve Clean Claim Submission Rates
Achieving consistently high clean claim rates requires systematic implementation of proven strategies across the entire billing workflow.
1. Prioritize Patient Registration Accuracy
Patient registration accuracy forms the foundation of clean claims, demanding meticulous attention to demographic details, insurance information, and contact data. Healthcare organizations must establish protocols for verifying patient identity, collecting complete insurance cards, and confirming policy details at every encounter.
2. Implement Real-Time Insurance Eligibility Verification
Insurance eligibility verification conducted in real-time prevents costly denials by confirming coverage status, benefit limitations, and prior authorization requirements before services are rendered. This proactive approach identifies potential issues such as inactive policies, coverage exclusions, or referral requirements that could compromise claim acceptance.
3. Align Documentation and Coding Practices with Specialty-Specific Requirements
Documentation and coding practices must align with specialty-specific requirements to ensure accuracy and compliance. Medical coders should receive ongoing training on current CPT codes, ICD-10 updates, and payer-specific guidelines. Regular audits of coding patterns help identify recurring errors and knowledge gaps that impact claim quality.
4. Integrate Technology for Enhanced Claim Accuracy
Technology integration through advanced EHR systems and automated billing software significantly enhances claim accuracy.
- Claim scrubbing tools: embedded within these platforms perform real-time validation checks, identifying missing information, coding inconsistencies, and formatting errors before submission.
- Automated error detection capabilities: reduce manual review time while ensuring comprehensive claim validation across multiple payer requirements and regulatory standards.
The Role of Specialized Medical Billing Services in Achieving Clean Claims
Outsourcing medical billing to specialized companies provides healthcare providers with dedicated expertise that internal teams often lack. Professional medical billing services employ certified coders who understand the nuances of specialty-specific requirements and maintain current knowledge of evolving payer policies across multiple insurance networks.
Claims scrubbing expertise represents a critical advantage of partnering with established billing companies. These services utilize sophisticated software systems that automatically detect coding errors, missing information, and compliance issues before claim submission. The multi- layered review process includes both automated validation and human oversight from experienced billing professionals.
Billing compliance support becomes particularly valuable as regulatory requirements continue to evolve. Specialized medical billing companies like Billing MedTech maintain dedicated compliance teams that monitor federal and commercial payer rule changes, ensuring claims meet current standards. This proactive approach reduces audit risks and maintains consistent reimbursement patterns.
The combination of specialized knowledge, advanced technology, and dedicated resources allows medical billing services to achieve clean claim rates that typically exceed 95%, compared to industry averages of 75-85% for practices managing billing internally.
Conclusion
The importance of clean claims in financial performance for healthcare providers cannot be overstated in today’s complex billing environment. Healthcare organizations that prioritize clean claim submission position themselves for sustained financial success while reducing operational inefficiencies that drain resources and impact patient care.
Clean claims serve as the foundation of effective revenue cycle management, directly influencing:
- Cash flow stability through faster reimbursement cycles
- Administrative efficiency by reducing denial management workload
- Compliance assurance that protects against costly audits and penalties
- Staff productivity through streamlined billing processes
Healthcare providers who invest in clean claim strategies, whether through internal process improvements or partnerships with specialized billing services, establish a competitive advantage that translates into measurable financial performance improvements and long-term practice sustainability.
Specialized medical billing services offer expertise in claims scrubbing, maintain compliance with billing standards, utilize advanced technology for accuracy, and
provide support throughout the billing process to enhance claim accuracy and maximize reimbursement efficiency.