Are you ready to grow up your business? Contact Us
Call us anytime
Are you ready to grow up your business? Contact Us
First-pass claim acceptance is a critical metric for medical practices seeking timely reimbursement and efficient revenue cycle management. A high first-pass acceptance rate ensures claims are paid without delays, reduces administrative burden, and strengthens cash flow. For U.S. doctors, understanding how to increase first-pass claim acceptance is not just a technical necessity—it is a strategic priority.
First-pass claim acceptance refers to the percentage of medical claims submitted to payers that are approved and processed correctly the first time. Claims rejected or denied on the first submission create delays, require resubmission, and increase operational costs. Maintaining a strong first-pass acceptance rate is especially important for solo practitioners and small to medium hospital practices where every delayed payment impacts financial stability.
A benchmark for many practices is achieving a first-pass acceptance rate of 95% or higher. However, this figure varies by specialty, payer type, and practice size. Understanding what drives denials is the first step to improvement.
There are several common reasons claims fail on the first submission. Errors in patient demographic information, incomplete insurance verification, and incorrect coding are leading causes. Documentation gaps, mismatched procedure codes, and eligibility issues often trigger automatic denials from payers. Some claims are rejected due to payer-specific rules or missing prior authorizations.
Identifying these denial patterns allows practices to implement preventive measures. Monitoring denial trends by payer or claim type also helps quantify the impact of errors on revenue and allows for targeted interventions.
Improving clean claims begins with accurate patient and insurance data. Practices should verify patient demographics, eligibility, and benefits before each visit. Front-desk staff must confirm insurance details and flag any inconsistencies. Coders and billing staff should ensure procedures are coded correctly according to the most recent CPT and ICD-10 guidelines.
Training and continuous education for staff on coding updates and payer rules is essential. Practices can also conduct periodic audits to catch errors early. By focusing on these preventive steps, medical offices can significantly improve their first-pass claim acceptance rates.
Revenue cycle management tools and claims scrubbing software have become invaluable for practices aiming to reduce denials. Claims scrubbing tools automatically check claims for errors, verify eligibility, and flag missing documentation before submission. Using these tools can reduce human error and increase the efficiency of billing workflows.
Automation through AI-enabled systems can provide predictive insights on likely denials, highlight high-risk claims, and suggest corrective actions. For practices considering outsourcing, partnering with experienced medical billing services can also improve clean claims and maintain a higher acceptance rate.
Tracking denial rates is a practical way to measure the effectiveness of first-pass claim improvements. By analyzing the reasons for denied claims and comparing them to industry benchmarks, practices can identify areas that need attention. Monitoring trends by payer, procedure, or coding error type allows teams to implement corrective actions quickly.
Benchmarking against peers or national averages provides context for performance. Regular reporting and feedback loops help ensure that improvements in first-pass claim acceptance are sustained over time.
Patient payments, copays, and deductibles can also influence claim acceptance. Clear communication with patients regarding their financial responsibility and timely collection of payments reduces the likelihood of claim rejections related to billing disputes. Accurate documentation of patient payments and balances ensures smoother processing with insurance providers.
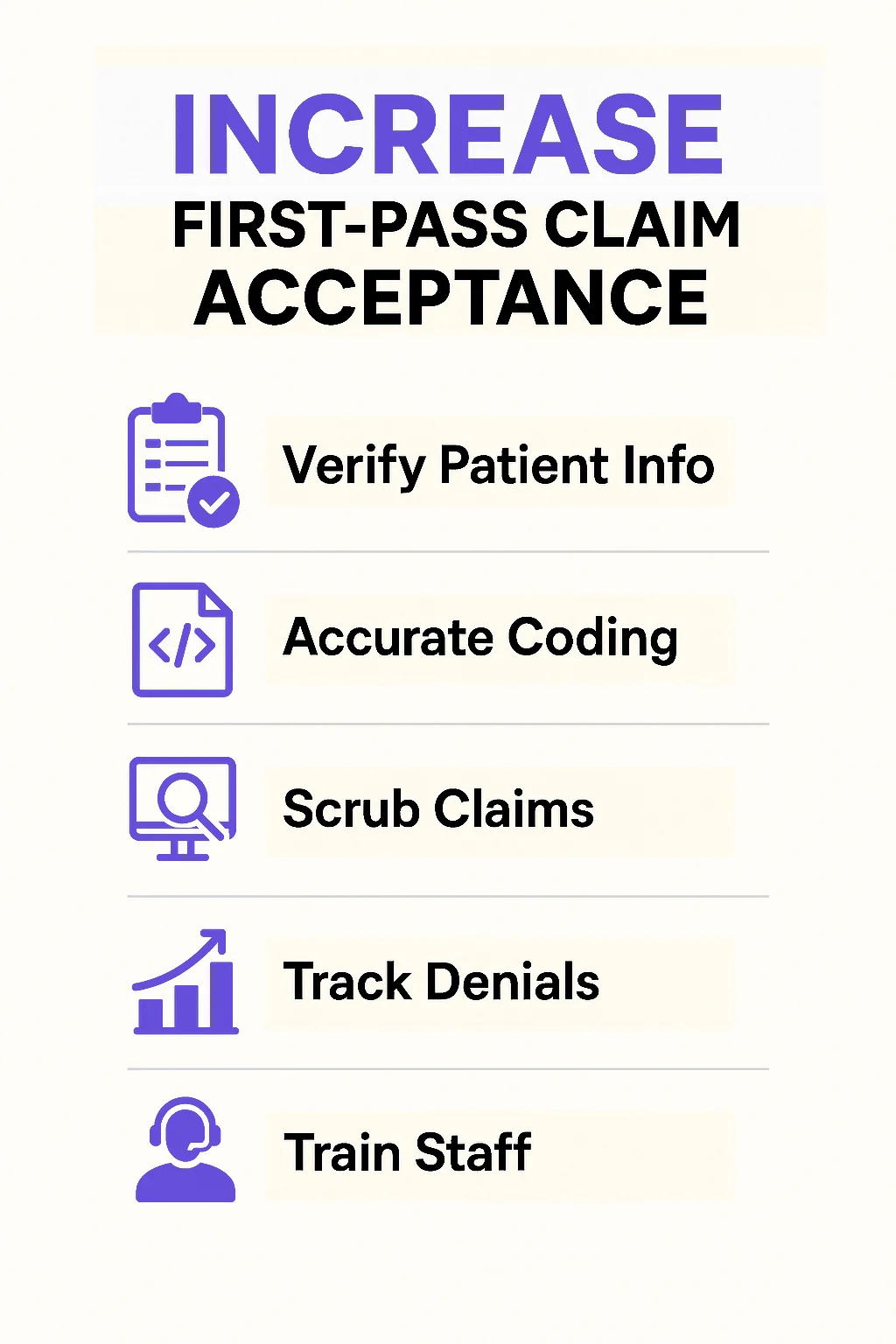
Increasing first-pass claim acceptance is a multifaceted process that involves accurate data entry, proper coding, payer-specific knowledge, and leveraging technology. Solo practitioners and large hospitals alike can benefit from focusing on clean claims, monitoring denial rates, and implementing workflow improvements. Using revenue cycle management tools, claims scrubbing software, and well-trained staff, practices can optimize revenue, reduce delays, and improve financial outcomes.
Arj Fatima is a certified medical billing and revenue cycle expert with 12+ years of experience helping U.S. healthcare providers optimize first-pass claim acceptance and reduce denials.
© Billing MedTech. All Rights Reserved