Are you ready to grow up your business? Contact Us
Call us anytime
Are you ready to grow up your business? Contact Us
CPT Code 66821 is used for YAG laser posterior capsulotomy. Correct billing depends on clear medical necessity, complete documentation, proper modifier use, and awareness of global period and NCCI bundling rules. Many denials result from poor symptom documentation, incorrect unbundling, or billing within the cataract surgery global period. Understanding Medicare and MAC expectations is critical to protect revenue and avoid audits.
If you perform a YAG laser capsulotomy, CPT Code 66821 appears straightforward.
In reality, it is one of the most frequently denied ophthalmology codes.
Most problems do not come from the procedure.
They come from documentation gaps, global period confusion, and modifier misuse.
Many practices lose payment quietly. Others face post-payment reviews months later.
This guide explains how to bill CPT Code 66821 correctly, using real-world billing experience from U.S. ophthalmology practices.
CPT Code 66821 describes laser treatment of the posterior lens capsule.
In simple terms, it is used when a patient develops posterior capsule opacification after cataract surgery. This clouding affects vision and requires treatment with a YAG laser.
This is not routine post-op care.
It is a separately billable procedure only when medical necessity is clearly documented.
Medical necessity is the most common reason CPT Code 66821 claims are denied.
Posterior capsule opacification must cause real functional vision problems. Mild haze alone is not enough. Medicare expects the chart to explain how the condition affects the patient’s daily life.
Symptoms such as reduced visual acuity, glare, difficulty reading, or trouble driving should be clearly documented. These symptoms must be tied directly to the patient’s complaint, not just listed as clinical findings.
A common documentation mistake is writing a short note such as, “PCO noted. YAG performed.” This language does not explain why the procedure was necessary at that time.
Experience-based insight:
In real audits, we see denials when symptoms are copied forward across visits without change. Medicare reviewers expect to see progression or functional impact, not repeated template language.
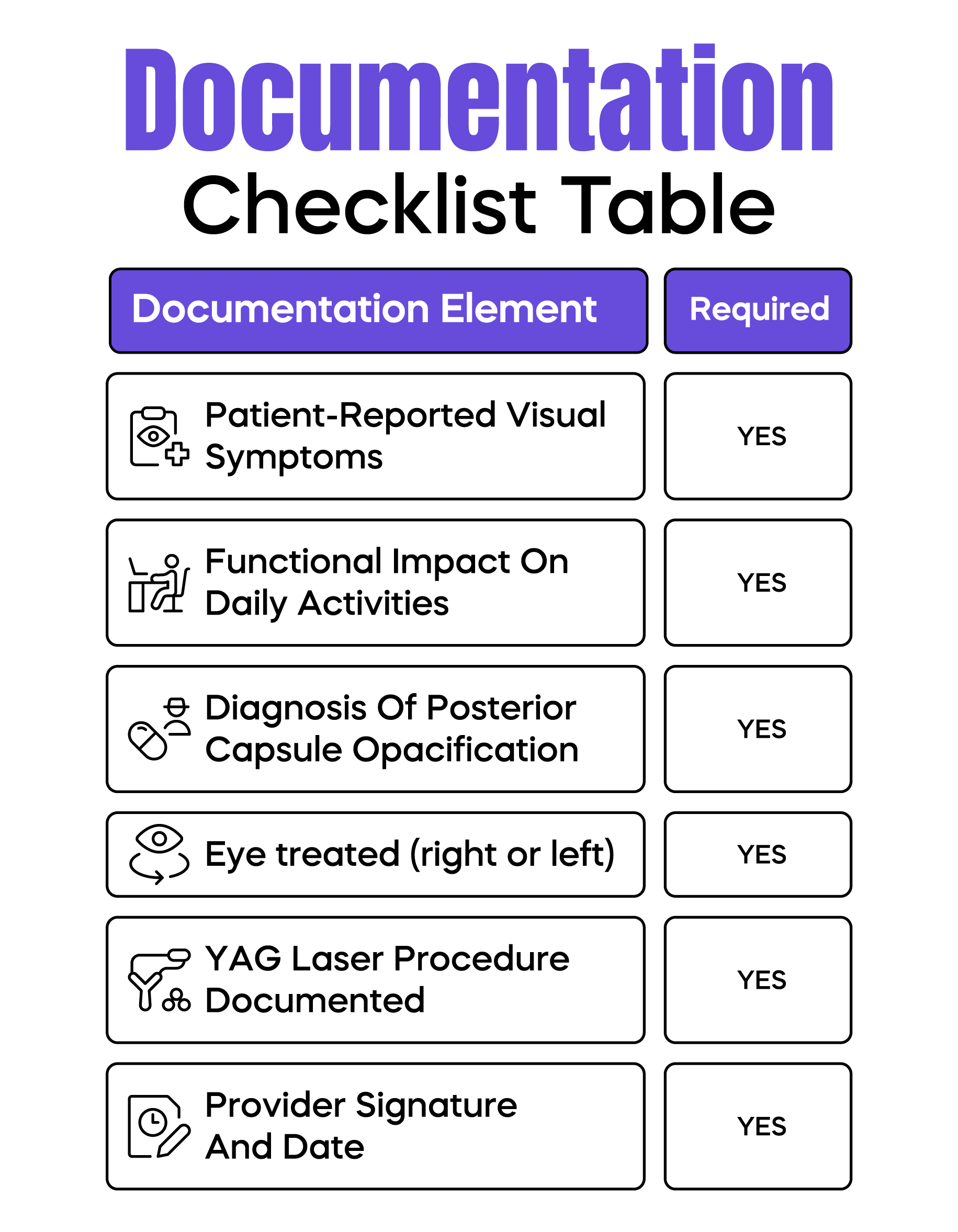
Documentation for CPT Code 66821 must clearly justify the procedure.
The medical record should explain the patient’s symptoms in plain terms and how those symptoms interfere with daily activities. The diagnosis of posterior capsule opacification must be clear and consistent throughout the note.
Laterality is critical. The chart must clearly state which eye was treated. Vague wording or missing laterality is a common reason for claim rejection.
The procedure itself should be documented with enough detail to show that a YAG laser capsulotomy was performed, along with the provider’s signature and date.
Real-world billing issue:
We frequently see denials when EHR templates auto-populate both eyes, but only one eye was actually treated. This creates inconsistencies that trigger payer reviews.
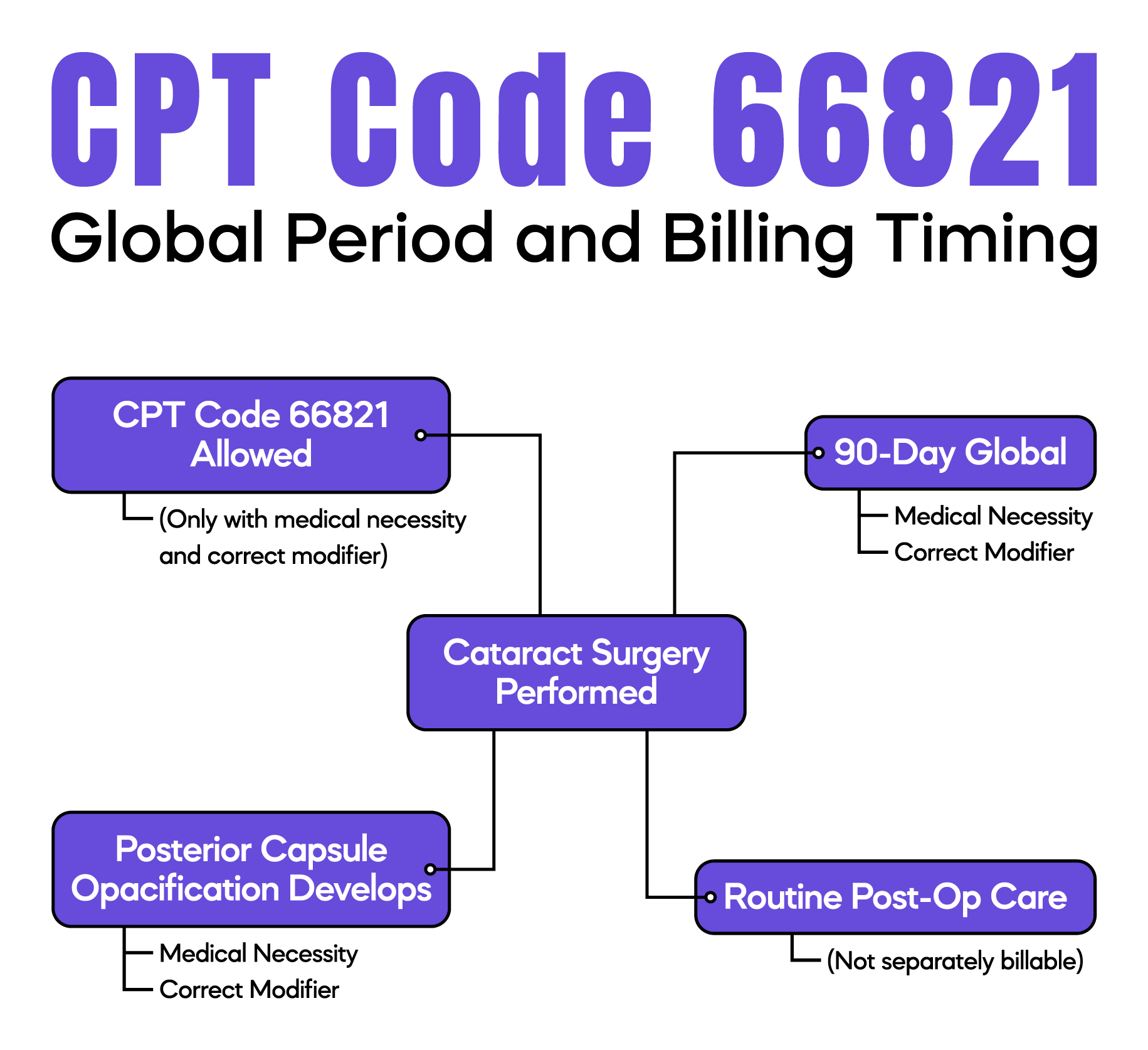
CPT Code 66821 carries a 90-day global period.
This becomes complicated because cataract surgery also has a global period. When posterior capsule opacification develops during that time, billing must be handled carefully.
Medicare may allow payment when the condition is not considered routine post-operative care. However, the medical record must clearly explain why the YAG procedure is separate from normal healing.
Some practices avoid billing entirely during the global period due to uncertainty. Others bill incorrectly and face recoupments months later.
Understanding how global periods overlap is essential to avoid both lost revenue and compliance risk.
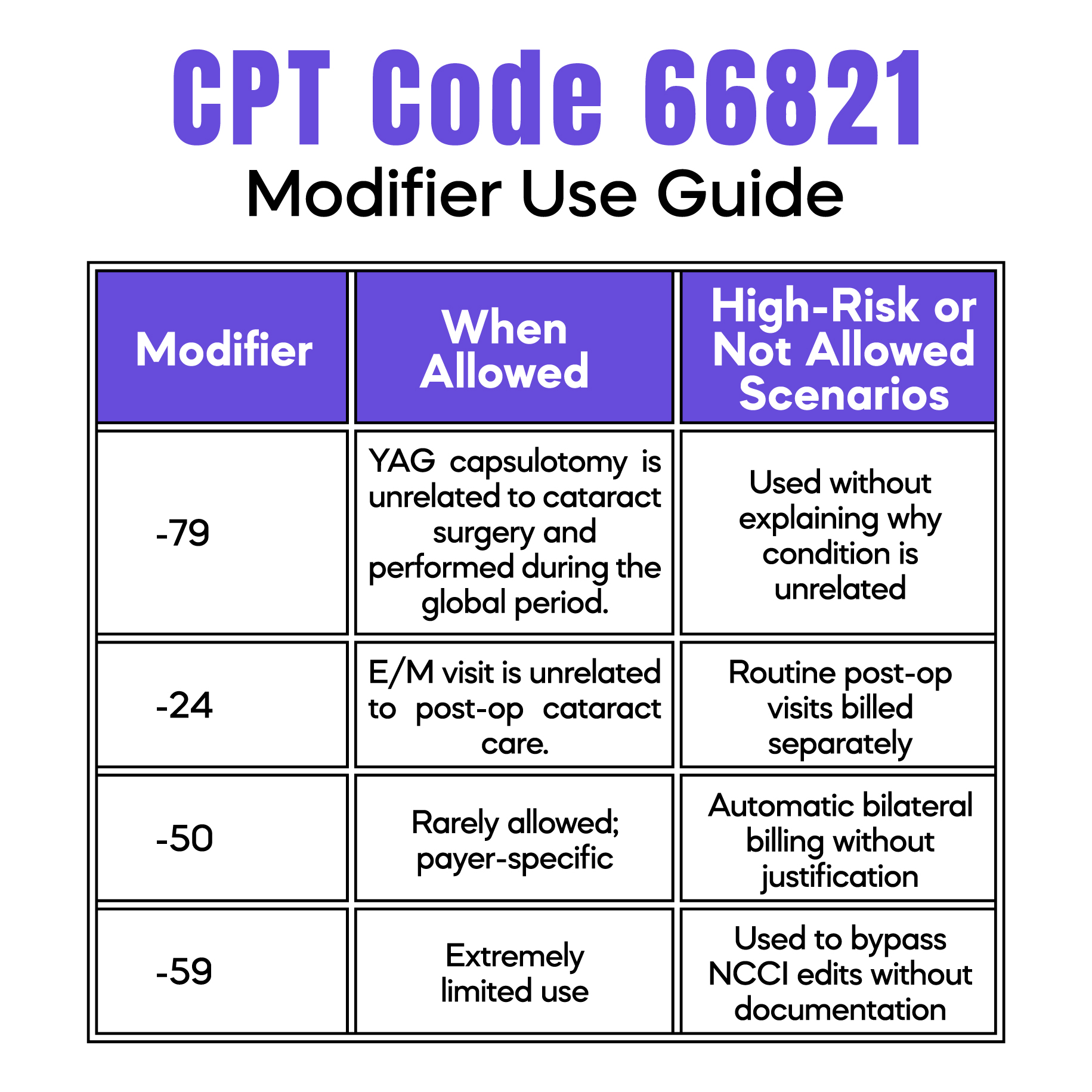
Modifier use must always be supported by documentation.
Modifier -79 may be appropriate when the YAG capsulotomy is unrelated to the original cataract surgery and performed during the global period. The note must clearly describe why the condition is new or separate.
Modifier -24 applies only when an evaluation and management service is unrelated to post-operative care. This modifier is often overused and closely reviewed by Medicare.
Modifier -50 is rarely appropriate for CPT Code 66821. Most payers expect the service to be billed per eye rather than as a bilateral procedure.
Audit insight:
We frequently see recoupments when modifiers are applied correctly from a coding standpoint but poorly explained in the medical record.
NCCI edits are a major reason CPT Code 66821 claims are denied.
This code is often bundled with cataract-related services, and unbundling is usually not allowed. Attempting to override NCCI edits without strong documentation increases audit risk.
Modifier -59 is rarely appropriate for CPT Code 66821. When it is used, the chart must clearly justify why the service is distinct and separately payable.
Billing warning:
Practices that rely on modifiers to bypass NCCI edits without explanation are more likely to face post-payment reviews.
Yes, but with limits.
You may bill CPT Code 66821 more than once when:
Billing the same eye repeatedly without clear progression increases audit risk.
Time gaps, symptom changes, and clinical reasoning must be documented.
Medicare Administrative Contractors (MACs) may apply different scrutiny levels.
Some MACs focus heavily on:
Local Coverage Determinations (LCDs) may outline specific expectations.
Practices should:
Most CPT Code 66821 denials follow predictable patterns.
Claims are denied when functional vision loss is not documented clearly. Billing during the cataract surgery global period without proper justification is another frequent issue.
Modifier misuse, especially automatic use of -24 or -79, raises payer red flags. Copy-paste EHR notes that show no change in symptoms also increase audit risk.
Each of these problems can be prevented with stronger documentation and internal claim reviews.
Strong billing for CPT Code 66821 starts with better documentation habits.
Symptoms should be documented using the patient’s own words whenever possible. The chart should clearly explain why treatment is needed at that visit, not just that posterior capsule opacification exists.
Practices should review modifier usage regularly and audit YAG laser claims to identify trends early. Staff education on global period rules can prevent both underbilling and overbilling.
Small workflow improvements often lead to significant reductions in denials and compliance risk.
Arj Fatima is a U.S. medical billing specialist with hands-on experience supporting ophthalmology and multispecialty practices. She focuses on CPT accuracy, Medicare compliance, denial prevention, and revenue protection. Her work reflects real-world billing challenges seen across U.S. practices, including modifier misuse, global period errors, and audit risk management. Arj writes educational content to help physicians bill confidently, stay compliant, and protect long-term revenue.
© Billing MedTech. All Rights Reserved