Are you ready to grow up your business? Contact Us
Call us anytime
Are you ready to grow up your business? Contact Us
Pediatric billing feels simple on the surface. Short visits. Healthy kids. Routine checkups.
But this is where many pediatric practices quietly lose revenue.
Most billing problems in pediatrics do not come from complex procedures. They come from small rule mistakes. A missed modifier. A wrong diagnosis link. A preventive visit coded incorrectly. An E/M level chosen without full documentation.
These errors rarely stop claims right away. Payments may still come in. But later, they show up as takebacks, denials, payer letters, or audit risk.
Pediatric billing and coding rules are strict because children are covered differently. Age rules apply. Preventive care schedules matter. Vaccines follow their own logic. Medicaid and commercial payers often apply different standards.
This guide explains pediatric billing and coding rules in clear language. It is written for U.S. pediatricians, solo practice owners, and decision-makers. The goal is simple. Help you bill correctly, get paid fully, and reduce compliance risk.
Pediatric practices operate on volume. Small payment differences add up fast.
A missed modifier on a combined preventive and sick visit can reduce payment by over 40 percent. An E/M level downcoded due to weak documentation can repeat hundreds of times a year. Vaccine administration errors can delay payment entirely.
In real practice, we often see this pattern. Claims are paid. No alerts appear. Then months later, a payer requests records. The issue is not fraud. It is a rule misunderstanding.
CMS, Medicaid programs, and commercial payers expect pediatric billing to follow very specific rules. When those rules are not followed, audits focus on patterns, not one-off errors.
Correct billing protects revenue. It also protects your practice from compliance stress.
Pediatrics is not adult medicine with smaller patients. Billing rules reflect that.
Age affects coding. Preventive care frequency is higher. Developmental screening is common. Vaccines dominate visits. Medicaid plays a larger role.
Adult billing often focuses on chronic disease management. Pediatric billing focuses on growth, prevention, and parental counseling. Documentation must reflect this difference.
Another key difference is visit overlap. Pediatricians frequently address acute problems during preventive visits. Billing rules allow this. But only when documentation is clear, and modifiers are used correctly.
Understanding these differences is the foundation of clean pediatric billing.
CPT codes describe the service you provide. In pediatrics, a small group of codes makes up most claims.
Most pediatric office visits use E/M codes from the 99202–99215 range. These apply to sick visits, follow-ups, and problem-focused care.
The correct level depends on either time spent or medical decision-making. For pediatrics, documentation often fails to support the chosen level, especially when visits feel routine.
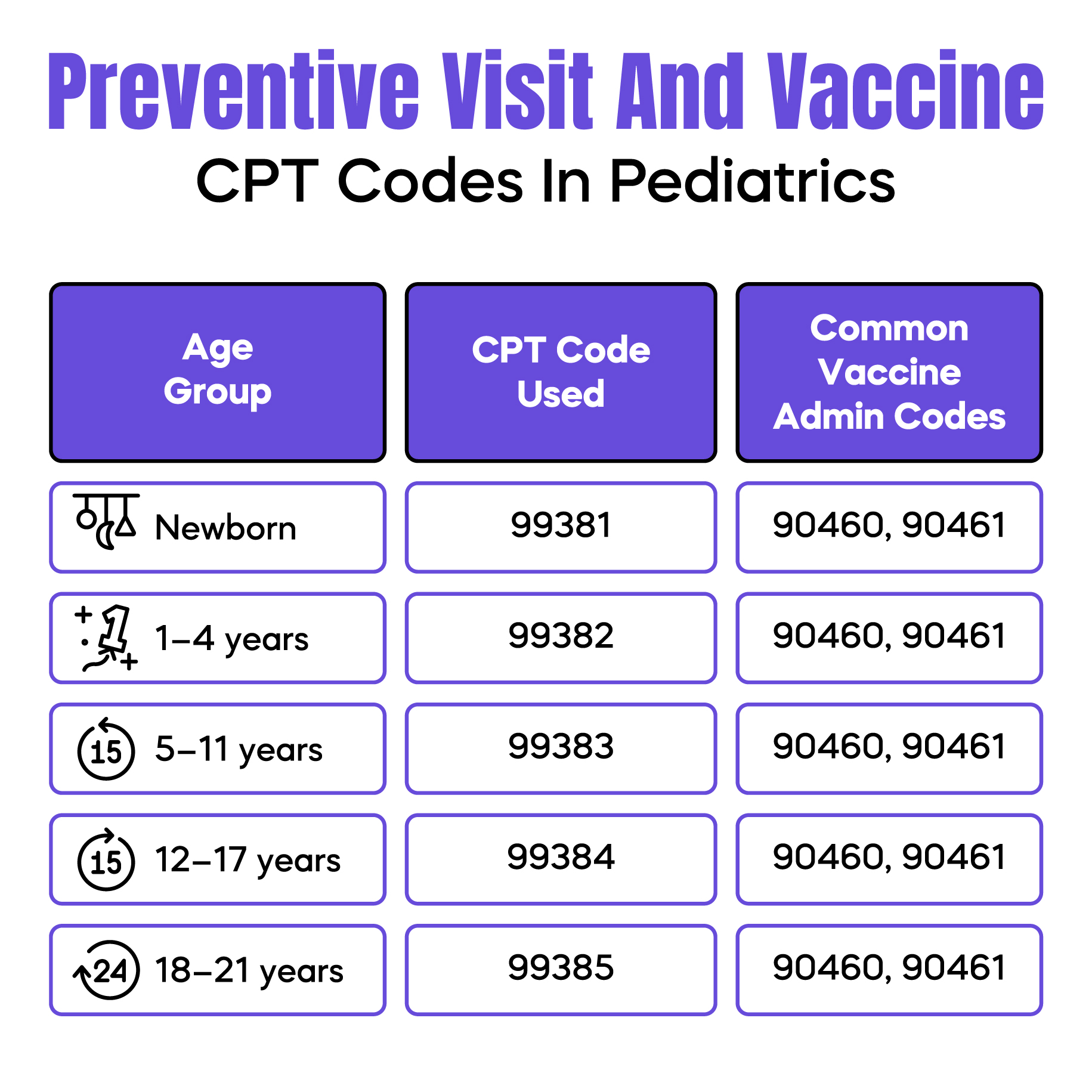
Preventive visits use age-based CPT codes such as 99381–99395.
These codes include counseling, anticipatory guidance, and age-appropriate screenings. They do not include treatment of acute problems.
This distinction matters. When a sick issue is addressed during a preventive visit, it must be documented separately.
Vaccines involve multiple codes. One for the product. One or more for administration.
Administration codes depend on counseling and patient age. Missing or mismatching these codes is a common reason for delayed payment.
Diagnosis codes explain why the service was needed. In pediatrics, ICD-10 rules are often misunderstood.
Some diagnosis codes are age-restricted. Others imply developmental stages. Using an adult-oriented diagnosis for a child can raise payer flags.
For example, developmental delays, feeding problems, and behavioral concerns require precise coding. Vague symptom codes increase denial risk.
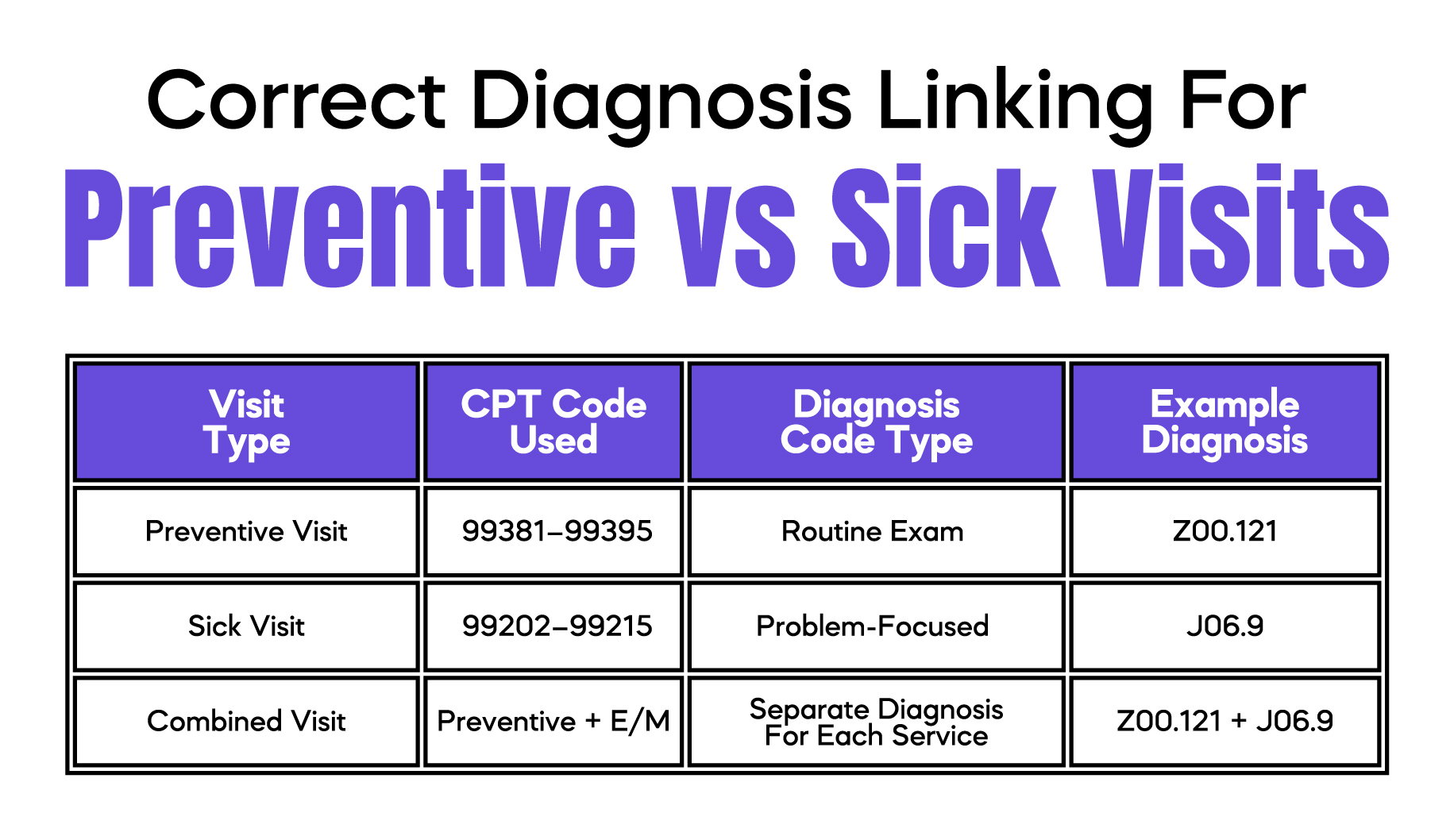
Every billed service must connect logically to a diagnosis. Preventive visit codes should link to routine exam diagnoses. Sick visit codes must link to problem-specific diagnoses.
One common error is linking a sick diagnosis only to the preventive visit code. This causes partial payment or silent downcoding.
Clear diagnosis linking protects both payment and compliance.
E/M coding is one of the most audited areas in pediatrics.
You can choose the E/M level based on time or on medical decision-making. Most pediatric visits rely on decision-making.
Decision-making depends on three factors. Problems addressed. Data reviewed. Risk level.
In pediatrics, risk is often underestimated. Managing asthma, infections, medication decisions, or parental concerns can raise the risk level when documented correctly.
A common real-world issue occurs when notes focus heavily on reassurance but not on clinical reasoning. The visit may deserve a higher level, but documentation does not support it.
Strong E/M documentation protects your payment and reduces audit exposure.
This is one of the most misunderstood rules in pediatric billing.
Preventive visits cover routine exams, growth tracking, and counseling. Sick visits cover evaluation and treatment of problems.
Both can be billed on the same day. But only when rules are followed.
To bill both visits, the sick problem must be significant and separately documented. A quick mention does not qualify.
Documentation must clearly separate preventive care from problem-focused care. The assessment and plan should reflect this separation.
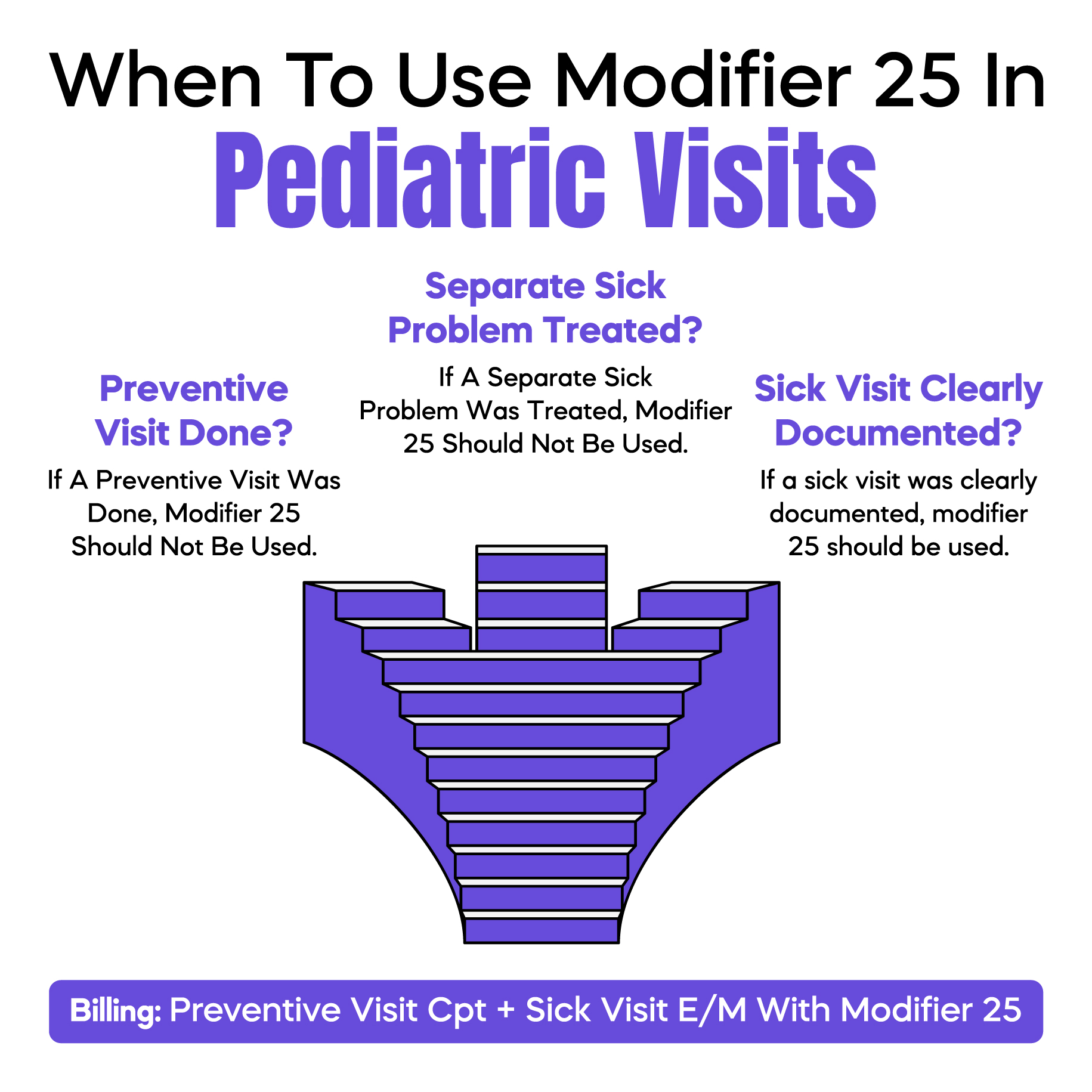
Modifier 25 is used to show that a significant, separate E/M service was provided on the same day as a preventive visit.
Modifier use without proper documentation is one of the top pediatric audit triggers. Payers look for patterns. Not individual claims.
Used correctly, modifier 25 protects payment. Used loosely, it increases risk.
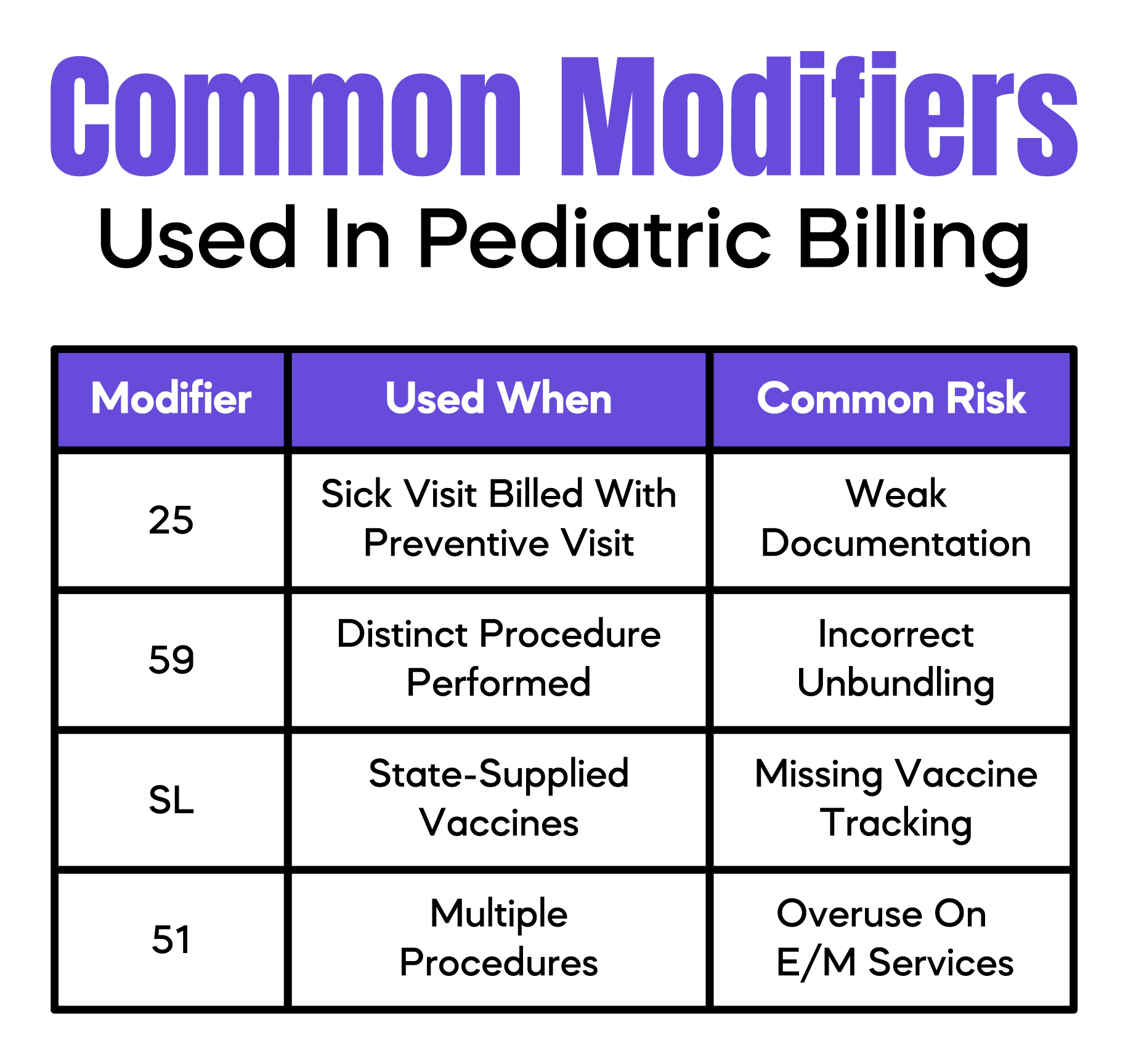
Modifiers explain special billing situations. In pediatrics, a few modifiers appear often.
Modifier 25 shows a separate E/M service on the same day as another service.
Modifier 59 is used to show distinct procedures when bundling rules would otherwise apply.
Vaccine-related modifiers may apply depending on payer rules.
The mistake many practices make is using modifiers defensively. Modifiers should explain documentation, not replace it.
Clear notes come first. Modifiers support the story your documentation already tells.
Most pediatric billing errors are small. But they repeat.
One common issue is undercoding sick visits because the visit felt quick. Another is overusing modifier 25 without strong documentation.
Vaccine administration errors are also frequent. Missing counseling documentation can reduce payment.
Diagnosis mismatches cause silent denials. Claims may pay partially without warning.
These errors often go unnoticed until revenue drops or an audit begins.
Pediatric audits focus on patterns.
Payers look at how often modifier 25 is used. They compare E/M levels across providers. They review vaccine billing consistency.
Medicaid audits are often retrospective. Commercial payers may request records months later.
Strong documentation and rule-based billing reduce audit stress. Clean billing is easier to defend.
Good pediatric billing starts in the exam room.
Document clearly. Separate preventive and problem-focused care. Link diagnoses correctly. Choose E/M levels intentionally.
Regular internal reviews help catch issues early. Education matters more than software.
Billing rules change. But strong fundamentals always apply.
Arj Fatima is a U.S. medical billing and compliance specialist with hands-on experience supporting pediatric, primary care, and multispecialty practices. She works closely with physicians to identify documentation gaps, reduce claim denials, and improve revenue without increasing audit risk. Her expertise includes CMS rules, CPT, and ICD-10-CM coding, modifier compliance, and payer-specific billing behavior across Medicare, Medicaid, and commercial insurers.
© Billing MedTech. All Rights Reserved