Are you ready to grow up your business? Contact Us
Call us anytime
Are you ready to grow up your business? Contact Us
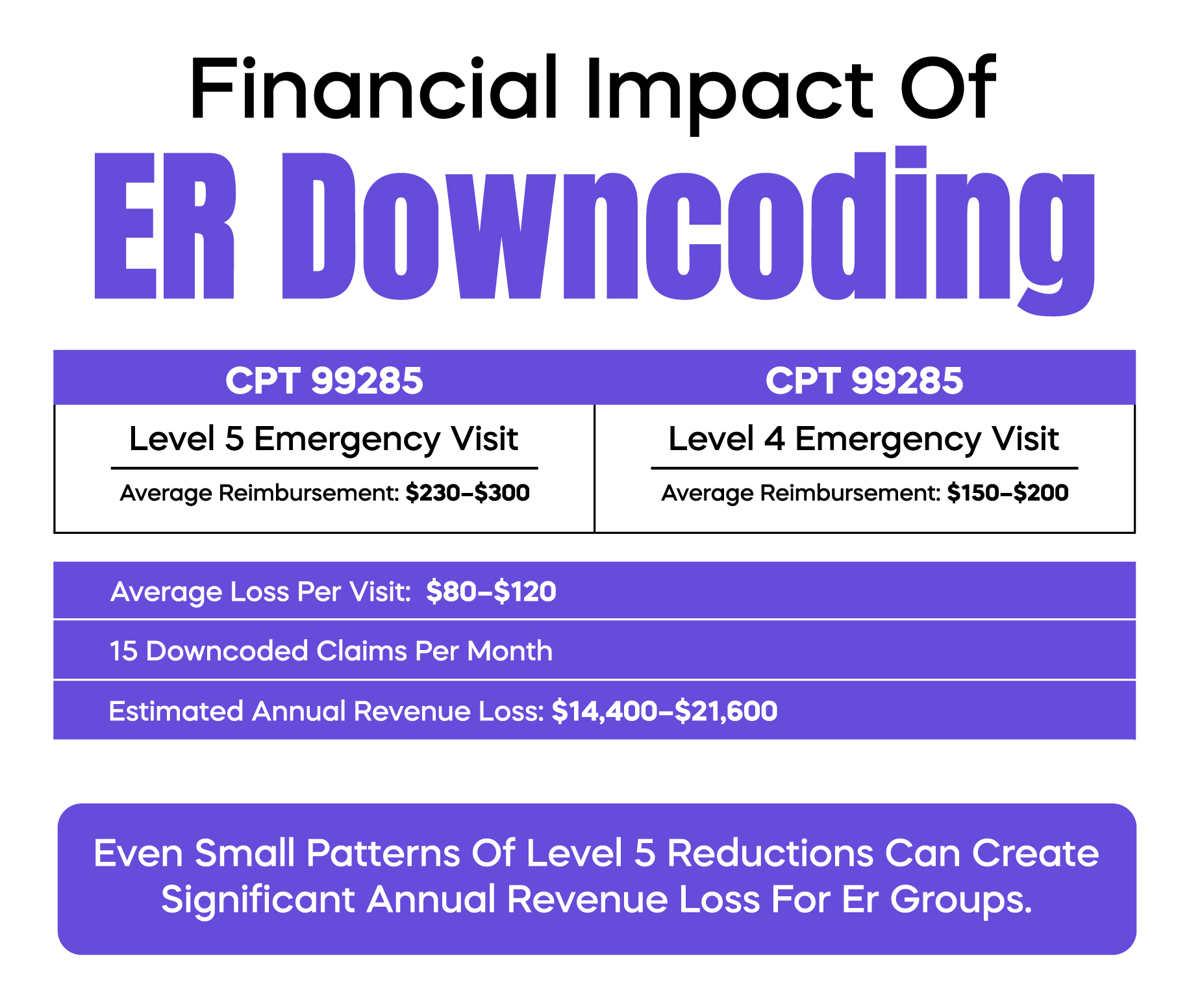
Emergency physicians and practice owners know the frustration of seeing high-level ER claims reduced by payers. A Level 5 visit (CPT 99285) can easily be downcoded to Level 4 (99284), cutting your reimbursement by hundreds of dollars per patient. Over a year, this adds up to thousands, or even tens of thousands, lost revenue.
Downcoding happens even when care is clinically appropriate. It often comes down to documentation gaps, payer review patterns, or automated audits. Understanding why it occurs and how to prevent it is crucial for protecting revenue and reducing audit risk.
This article walks you through real-world ER scenarios, common mistakes, prevention strategies, and step-by-step appeal guidance.
ER downcoding is when a payer lowers the E/M level of your submitted emergency visit claim. For example, you submit CPT 99285 for a high-complexity patient, but the insurance company pays at 99284 or lower.
Downcoding can happen with Medicare, Medicaid, or commercial payers. While CMS rules are more transparent, commercial payers often use proprietary algorithms that flag high-level claims.
Incomplete documentation: Missing History of Present Illness (HPI), Review of Systems (ROS), or exam elements.
ICD-10-CM mismatch: Diagnosis codes must justify the level of service. If the code doesn’t match complexity, payers may reduce the claim.
Time discrepancies: Documented time doesn’t align with typical CPT expectations for high-complexity visits.
Modifier misuse: Incorrect use of Modifier 25 can raise payer scrutiny.
CMS-1500 submission errors: Incorrect fields can automatically trigger downcoding or denial.
Example: A patient with sepsis receives high-level care. CPT 99285 is submitted, but only a brief exam is documented. The claim is downcoded to 99284. The practice loses $200–$300 per visit.
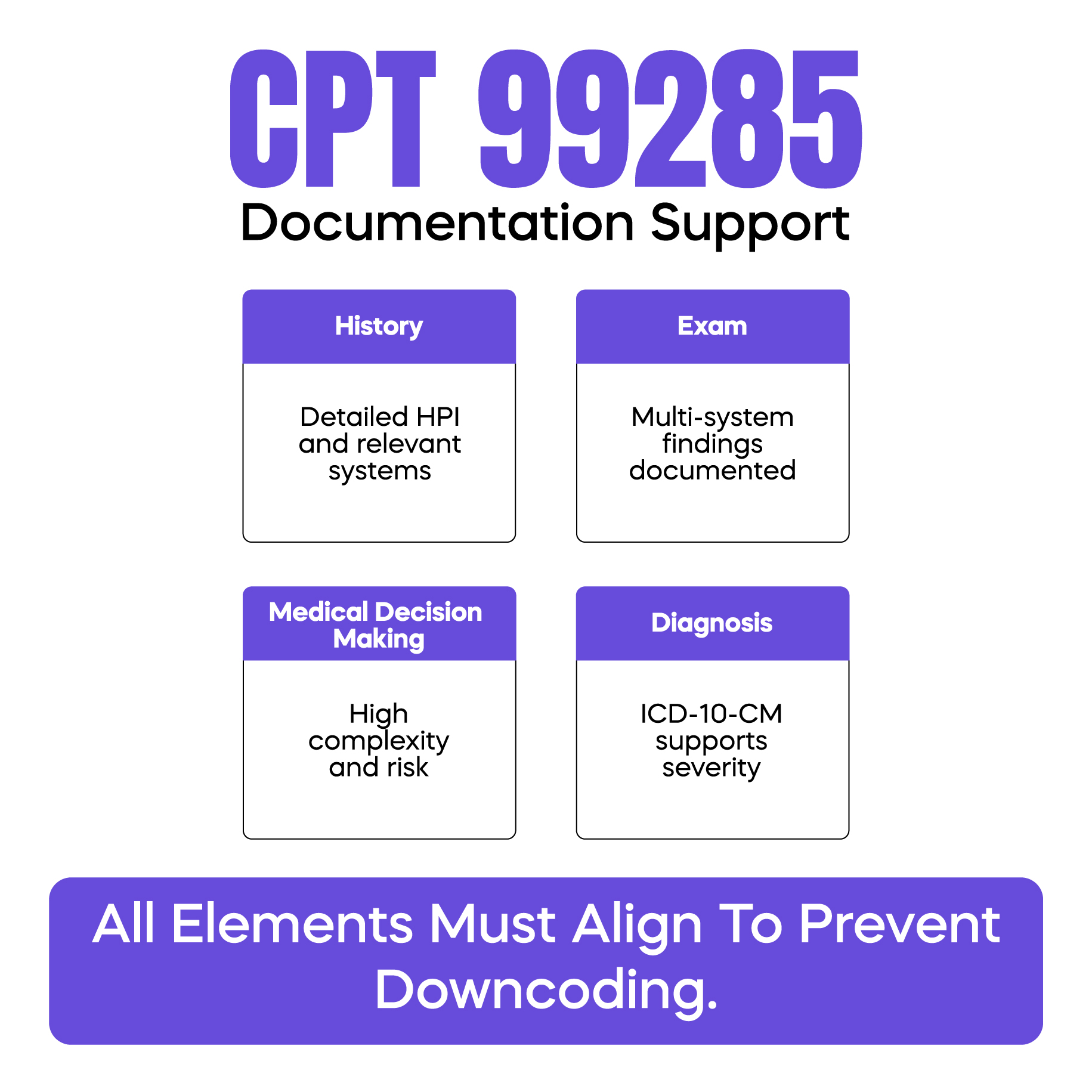
Even experienced physicians can be affected by downcoding. Errors that commonly trigger reductions include incomplete history, such as missing details in the History of Present Illness or Review of Systems, and insufficient physical examination documentation. For a 99285 claim, the exam must cover at least eight organ systems or two extended exams. Choosing the wrong CPT code under time pressure is another frequent error, as is incorrect use of Modifier 25, which is intended only for separate, significant services performed on the same day. Submission errors on the CMS-1500 form, such as misplaced ICD-10-CM codes or missing diagnosis pointers, also contribute to downcoding. The critical principle is that the CPT code, diagnosis, and documentation must align. If the chart does not demonstrate medical necessity and complexity, the payer will reduce the payment.
Payers determine the appropriate ER level using a combination of automated algorithms and manual review. Automated systems look for mismatched diagnoses, missing exam or history elements, and patterns that differ from typical Level 5 claims. For Medicare, Local Coverage Determinations and MAC audits play an additional role, reviewing charts to ensure documentation supports the billed CPT code. Commercial payers often operate with less transparency, flagging claims based on historical billing patterns or outlier submissions. For example, if a physician repeatedly bills 99285 for chest pain coded as R07.9 without detailed exam notes, future claims may be automatically downcoded. Understanding how payers evaluate claims is crucial to preventing revenue loss.
Preventing downcoding requires a combination of careful documentation and proactive auditing.
1. Use an ER-specific documentation checklist:
| Required Element | Level 5 CPT Requirement |
|---|---|
| HPI | ≥4 elements or extended narrative |
| ROS | ≥10 systems or extended |
| Physical Exam | ≥8 organ systems or extended exam |
| Medical Decision Making | High complexity |
| Time | Documented if time-based billing |
2. Link ICD-10-CM codes properly:
Ensure the diagnosis justifies the complexity. For example:
Chest pain (R07.9) with EKG and lab review supports 99284, but may need additional findings for 99285.
3. Track time accurately:
Document time spent on patient care if using time-based billing. Include counseling and coordination.
4. Conduct pre-submission audits:
Identify claims with missing exam elements or inconsistent coding.
Correct issues before submission to avoid downcoding.
5. Use EHR templates and prompts:
Smart prompts can remind physicians to include necessary HPI, ROS, and exam details for Level 5 visits.
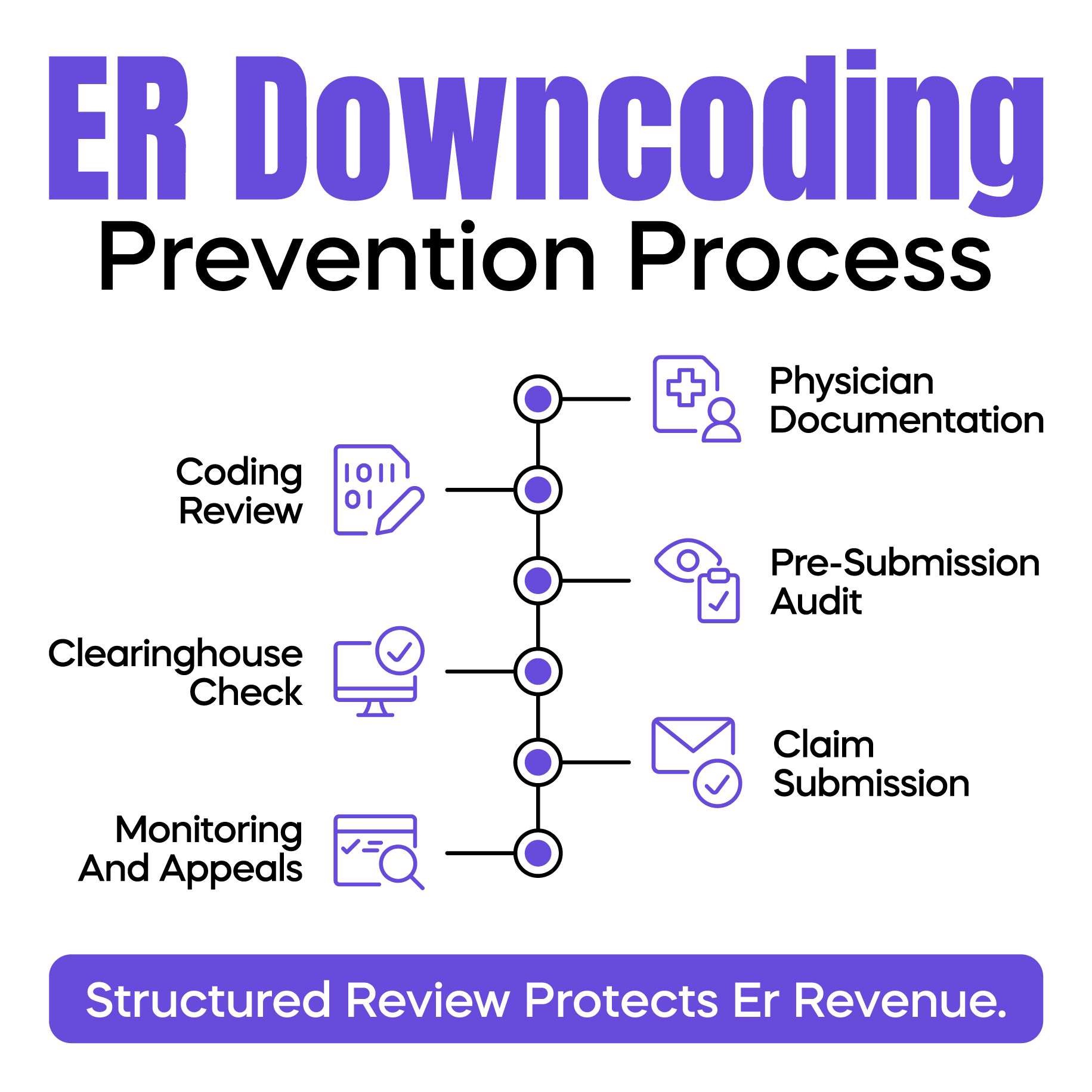
Even with prevention, some claims will be downcoded. A structured appeal process helps recover revenue.
Step-by-step appeal workflow:
Step 1: Identify the downcoded claim and gather the payer's explanation.
Step 2: Review documentation against CPT 99285 requirements.
Step 3: Draft an appeal letter emphasizing:
Step 4: Attach supporting records:
Step 5: Submit within the payer deadline and track the response.
Step 6: Escalate to peer-to-peer review if the initial appeal fails.
Tip: Include specific examples of patient complexity. Payers respond best to concrete documentation, not general statements.
Modern ER practices can use technology to minimize the risk of downcoding. EHR templates designed for Level 5 visits help ensure all required documentation elements are captured. Clearinghouse edits can flag potential downcoding issues before claims are submitted, allowing correction before payment reduction occurs. Revenue cycle management systems can generate alerts when claims deviate from typical payer patterns, highlighting visits that may be at higher risk. A structured workflow, where physicians document using templates, the coding team reviews for completeness, clearinghouse edits are applied, and revenue cycle alerts monitor unusual denials or downcodes, can significantly reduce the risk of lost revenue.
Protecting ER revenue requires ongoing vigilance, not one-time fixes. Implementing structured workflows can prevent thousands of dollars in lost revenue annually.
Arj Fatima is a U.S.-based medical billing expert specializing in emergency department coding, revenue cycle management, and CMS compliance. With years of experience supporting physicians and ER practices, Arj provides practical, doctor-focused strategies to prevent denials, reduce audit risk, and optimize revenue.
© Billing MedTech. All Rights Reserved